Lessons from Smart Hospital Activations
What We Can Learn from Houston Methodist’s Cypress Hospital
Healthcare construction is evolving quickly. The idea of the “smart hospital” is no longer futuristic. It is here, and it is reshaping how facilities are designed, built, and activated.
At the Blueprints & Breakthroughs: Strategies for Smarter Healthcare Construction panel, Maggie Duplantis, Director of Clinical Planning and Design at Houston Methodist, and Timothy Menz, Assistant Vice President of Transition Planning at Northwell Health, shared their perspectives on activating technology-rich facilities. Their lessons highlight both the opportunities and the challenges of blending advanced infrastructure with human-centered
What Makes a Hospital “Smart”
Smart hospitals integrate digital and automated systems into nearly every aspect of operations.
Houston Methodist’s Cypress Hospital, opened in March, included:
· Advanced nurse call systems linked to mobile devices
· Smart patient rooms with adaptive lighting, climate, and entertainment controls
· Real-time location systems (RTLS) for equipment, staff, and patients
· Digital wayfinding and patient education displays
· Building systems that monitor energy use and air quality in real time
As Duplantis explained, “It’s not just lights, booms, and beds anymore. It’s the network, the software, and how everything talks to each other.”
Activation Lessons Learned
Involve Technology Teams from Day One
Technology underpins nearly every system in a smart hospital, from medical equipment to patient engagement tools. That’s why IT can’t be an afterthought it has to be at the table from the beginning.
Menz stressed this point clearly: “If you’re not thinking about how the equipment and the network work together early, you’re already behind.”
Duplantis echoed the importance of early alignment, adding: “Without IT’s input, you’re setting yourself up to miss critical infrastructure.”
Plan for a Steeper Training Curve
The transition to smart hospital systems doesn’t just bring new tools it forces staff to unlearn habits built over years of practice. At Cypress, even something as simple as answering a patient call required a completely new workflow.
Duplantis explained the challenge: “When you change how a nurse answers a call, you’re changing muscle memory that’s been in place for decades.”
For Menz, the solution is repetition and simulation: “One class isn’t enough. We run repeat sessions and simulations so staff feel confident before patients arrive.”
Align Vendors to Prevent Delays
Complex projects require open and continuous communication across multiple vendors. Vendors often have to coordinate across specialties. An example would be medical equipment, which now has to integrate into the network, forcing both the medical equipment and IT teams to collaborate.
Duplantis explained, “If you don’t have vendors talking to each other, you’re setting yourself up for finger-pointing and delays.”
Menz echoed the challenge, saying, “Even with something as basic as equipment deliveries, if you don’t have proactive coordination, it falls apart fast.”
Build Extra Time for Testing and Validation
Traditional hospital activations often stop at making sure equipment powers on. But in a smart hospital, the real work comes in confirming that all the digital integrations function seamlessly together.
Menz cautioned against leaving this to the last minute: “On one project, we were testing integrations the week before opening. That’s not where you want to be.”
Duplantis described the depth of testing required: “It’s not enough to see the button light up — we had to confirm alerts went to a phone, showed up on a board, and logged in the record.”
Support Staff After Opening
The complexity of smart hospitals doesn’t end on opening day. The first few weeks are often the most critical, as staff adapt to new systems while caring for patients in real time. On-the-ground support can make or break that transition.
At Houston Methodist, Duplantis saw the difference this made: “We had technology support right on the units, answering questions on the spot. That made all the difference.”
Menz shared a similar strategy at Northwell: “We put roving support teams on the floors so staff didn’t feel abandoned.”
How FitUp Can Help Solve These Challenges
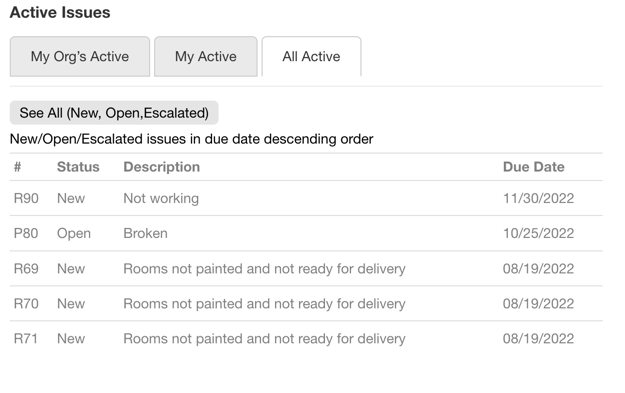
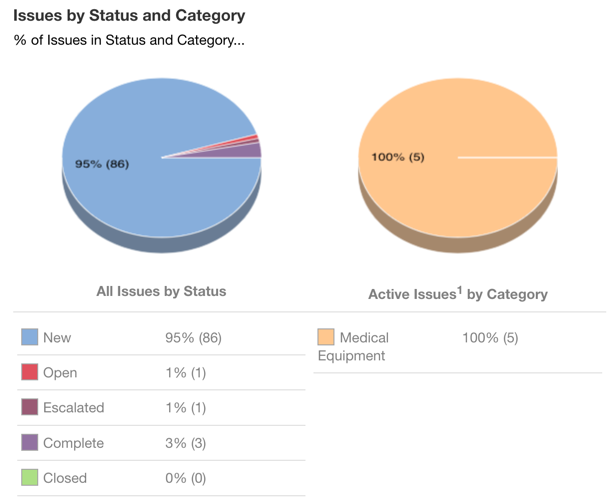
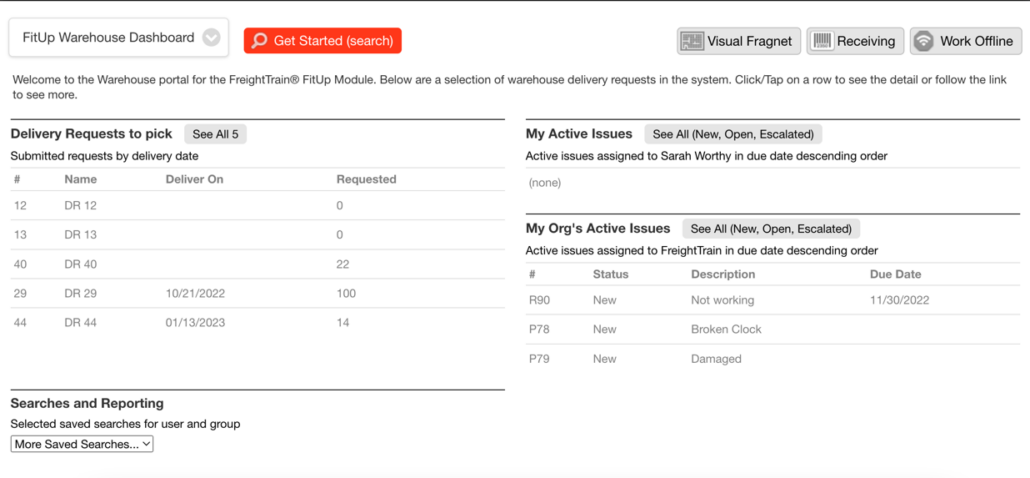
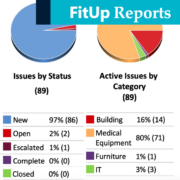
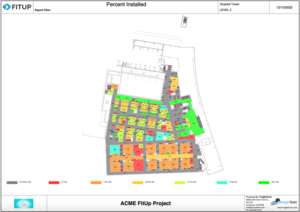
The lessons from Houston Methodist’s recently opened Cypress Hospital highlight a common theme: complexity multiplies when multiple systems, vendors, and workflows must align. This is exactly where FitUp provides value.
FitUp was designed to streamline hospital activations by giving project teams a single source of truth. Instead of relying on scattered spreadsheets, endless email chains, and siloed vendor updates, teams can manage equipment, IT, facilities, and training tasks all in one platform.
· Early Involvement of IT and Facilities: FitUp makes it easy to bring every stakeholder into the process from day one. Shared dashboards ensure that IT requirements aren’t overlooked and that infrastructure is planned in parallel with equipment and construction.
· Training Visibility: With task tracking and role-specific workflows, leaders can confirm that staff training milestones are complete and identify where additional support is needed before go-live.
· Vendor Coordination: FitUp eliminates finger-pointing by aligning vendors on shared timelines and deliverables. Everyone sees the same data, reducing delays caused by miscommunication.
· Testing and Validation: Teams can document and track validation steps directly in FitUp, ensuring that every system integration is tested and verified before patients arrive.
· Go-Live Support: Post-activation, FitUp’s real-time updates help leaders quickly respond to issues, track progress, and ensure staff aren’t left without the tools or support they need.
By making complex activations more transparent and collaborative, FitUp helps healthcare organizations focus less on chasing down details — and more on delivering safe, efficient, patient-centered care.
The Bigger Picture
Smart hospitals promise efficiency, improved patient experiences, and safer care, but they also add layers of complexity. Both leaders agreed that success requires:
· Early involvement of IT and facilities teams
· Extended training that reshapes workflows
· Structured vendor collaboration
· Extra time for testing and validation
· Visible support during the first days of operation