The Dangers of Cost Cutting in Healthcare Construction: When Saving Money Costs More
Controlling costs is always a priority in healthcare construction. However, when cost-cutting efforts compromise quality, the long-term financial and operational consequences can far outweigh the initial savings. Value engineering—re-evaluating project scope and materials to reduce expenses—can sometimes lead to expensive fixes down the road when not done properly or when the facility operational team is not included in key decisions.
In a recent webinar, industry experts shared real-world examples of cost-saving decisions that backfired, along with strategies to make better-informed choices.
1. Cutting Corners on HVAC Systems: A Costly Mistake
The HVAC system is one of the most critical yet frequently undervalued aspects of healthcare construction. Proper temperature control is essential for patient comfort, infection control, and equipment longevity. In one instance, a project team opted for a lower-cost HVAC system without fully evaluating its impact.
“A print shop in the facility had its thermostat in the wrong location, leading to drastic temperature fluctuations,” recalled Liz Callahan, Executive Director at City of Hope. “As a result, patient care areas were freezing whenever the print shop heated up.”
The fix required costly rework, including HVAC system modifications and moving staff to temporary offices. What seemed like a minor budget cut ended up causing major operational disruptions and additional expenses.
2. Eliminating Essential Safety Features
In another case, a decision to remove patient-assist bars next to toilets in a hospital hotel created a major patient safety issue.
“Nursing staff quickly flagged this as a problem,” said Callahan. “Without these bars, fall risks increased significantly, and we had to install them after the fact—at a much higher cost.”
Beyond the unexpected cost of installation after project was complete, this oversight posed a liability issue and delayed the facility’s readiness. Safety features should never be considered an optional expense, as patient well-being is at stake.
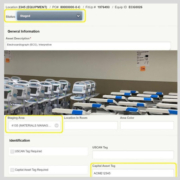
3. Room Numbering Mishaps: A Half-Million-Dollar Fix
Something as simple as room numbering can have significant cost implications. John Stiles from Ohio State University Wexner Medical Center shared an example where room numbering inconsistencies across different systems led to an expensive correction.
“We had a four-digit room numbering system in one tower and a five-digit system in another. The result? A half-million-dollar budget hit to standardize and update all related systems.”
To prevent such errors, coordination across IT, facilities management, and clinical operations is essential early in the project planning phase.
4. The Hidden Costs of Value Engineering
Value engineering is often necessary, but it should be approached strategically. Cutting costs in the wrong areas—such as IT infrastructure, security, or accessibility—can lead to major setbacks. Corey M. Gaarde, a healthcare IT expert, emphasized the importance of evaluating long-term operational impact when making these decisions.
“It’s not just about upfront savings,” Gaarde said. “If you don’t account for future technology integrations, you could end up with outdated or inefficient systems that require expensive retrofits.”
Best Practices for Smart Cost Reduction
Instead of making short-sighted cuts, consider these best practices to balance cost efficiency with quality:
- Involve the Right Stakeholders Early – Ensure clinicians, IT specialists, and facility managers are part of budgeting discussions from the start.
- Analyze Long-Term Costs – Consider life cycle costs, not just upfront expenses. Cheaper solutions may require costly replacements sooner.
- Set Clear Priorities – Define essential features that should not be compromised, such as patient safety, technology integration, and HVAC reliability.
- Use a Structured Change Request Process – Implement a governance structure to evaluate cost-cutting proposals and assess risks before making decisions.
Final Thoughts: Investing in Quality Saves Money in the Long Run
Cutting costs in healthcare construction is necessary, but it must be done strategically. When savings come at the expense of functionality, safety, or long-term efficiency, the financial burden can far exceed the initial reduction. By planning for hidden costs, engaging the right stakeholders, and considering long-term implications, healthcare organizations can achieve both financial and operational success.